During the course of a great telephone conversation with a migraine headache patient from San Diego last week, it once again became evident to me that there is a misunderstanding of the differences in nerve blocks and Botoxinjections done by surgeons vs other medical professionals when it comes to the treatment of Migraine Headaches and Occipital Neuralgia. The differences can be broken down into three different categories:
Why the injections are performed…
What is injected….
Where it is injected…
Let’s talk about all three.
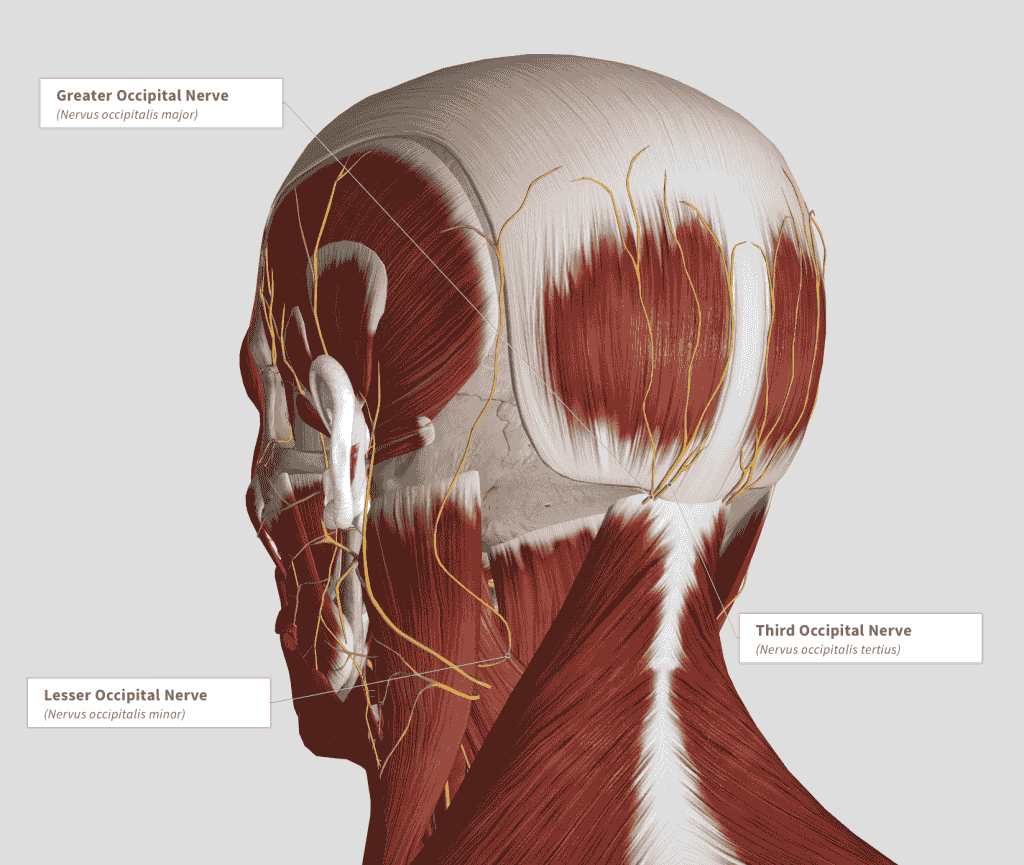
First let’s address the WHY. When I inject a patient for a workup for migraine surgery, I am doing that with the intent to numb the nerve in question for a short period of time. It is a DIAGNOSTIC injection, meaning that the purpose of the injection is not to provide long term relief. It is instead to see if numbing a specific nerve decreases the pain of the patient’s migraine headache. If the injection works and does decrease the migraine pain, then that is an indication that surgery on that nerve will likely provide long term relief. This is in contrast to a THERAPEUTIC injection done by neurologists or pain management doctors. The purposes of these injections are not to demonstrate that the nerve is the cause of the headache, but instead to decrease inflammation of the tissues around the nerve in the hopes that this will result in less nerve aggravation and less migraine pain.
This leads to the next difference which is WHAT is injected. My DIAGNOSTIC injections are a combination of short and medium term anesthetics. These drugs are meant to numb the nerve within five minutes and have an effect last for about four hours. If the nerve responds as expected, the patient’s headache pain decreases almost immediately and this relief lasts for four hours. Patients who experience this effect should have an excellent response to surgery. When neurologists and pain physicians perform nerve blocks, the main ingredient used is often a steroid, mixed with some short term anesthetic. The purpose here is to have the steroid decrease inflammation in and particularly around the nerve. If the steroid works, inflammation can be controlled for weeks to a few months and this may have a beneficial effect on improving the migraine headache pain. Patients who respond to this treatment are also likely to benefit from surgery, BUT PATIENTS WHO DO NOT RESPOND TO STEROID INJECTIONS MAY STILL VERY LIKELY BE SURGICAL CANDIDATES. Steroid injections are not diagnostic and so they are not a substitute for our DIAGNOSTIC injections.
Now it is also a bit confusing because both surgeons as well as neurologists and pain management physicians sometimes inject Botox. Botox is a muscle relaxer, and the purpose of Botox is not to numb the nerve but to relax the tissue around the nerve, decreasing pressure on the affected nerve in the hopes that this ‘medical decompression” will mimic the decompression we do with surgery. If this works, it will decrease the nerve irritation that causes the migraine headache. When done by a neurologist or pain doctor, Botox is most often injected all around the head and neck of a migraine patient. This “shotgun” approach is done in the hopes that one of these injections affects an area around a nerve that contributes to the patient’s migraine headache, and this often does work. Often, however, it does not work, but here again A BOTOX INJECTION BY A NON-SURGEON DOES NOT MEAN THAT A MIGRAINE PATIENT WILL NOT RESPOND TO BOTOX WHEN A SURGEON INJECTS IT.
There is a significant difference in my Botox injections, which leads us to the WHERE issue in the discussion. When I inject botox I do so in a very directed fashion, only around the nerves suspected to be instrumental in producing the migraine pain. By first doing a DIAGNOSTIC nerve block as discussed two paragraphs above, we can map out which nerves are the culprit in causing the migraine pain. By then applying Botox around those nerves, we can relax the tissue around the nerves in order to provide decompression that lasts for up to several months. Because surgeons such as myself have actually seen these nerves in surgery, we have a detailed understanding on where to find them and how to direct our Botox injections to the right spots. This is why injections by a migraine surgeon can work even when previous injections by other practitioners did not.
There is much more to discuss with respect to diagnostic injections, therapeutic Botox injections, and their relationship to surgery and more permanent results. That is a lot of what we do in consultations, and I spent an hour on the phone with last week’s migraine headache patient from San Diego discussing these very things. She has has had many injections by several different non-surgeons, and some of them worked though most of them did not. This is likely because the doctors doing the injections hit the right spot once or twice, but without the directed targeting that we do as surgeons, they missed the right spot the other times. This particular patient is very likely an excellent surgical candidate, and though she lives about 5 hours away, I’m looking forward to seeing her at her consultation visit so we can prove that relief from her migraine pain is likely obtainable.