In answering questions from Facebook groups and patients here in the office, it is becoming clear to me that many migraine sufferers may not understand that there is a BIG difference between cervical decompression surgery and the type of nerve decompression that we migraine surgeons perform in order to provide migraine relief.
What is Cervical Spine Disease?
The diagnosis of cervical spine disease is very common, both in and outside of the world of migraine headaches. Issues in the cervical spine can come from degeneration of bone, issues with arthritis, trauma, or other processes. When these issues occur, there can be compression on the nerve root, were the spinal cord branches off before individual nerves are formed. The nerves that come from these nerve roots can cross and combine before creating an end nerve that performs a specific function, such as providing sensation to the scalp in the case of the greater occipital nerve.
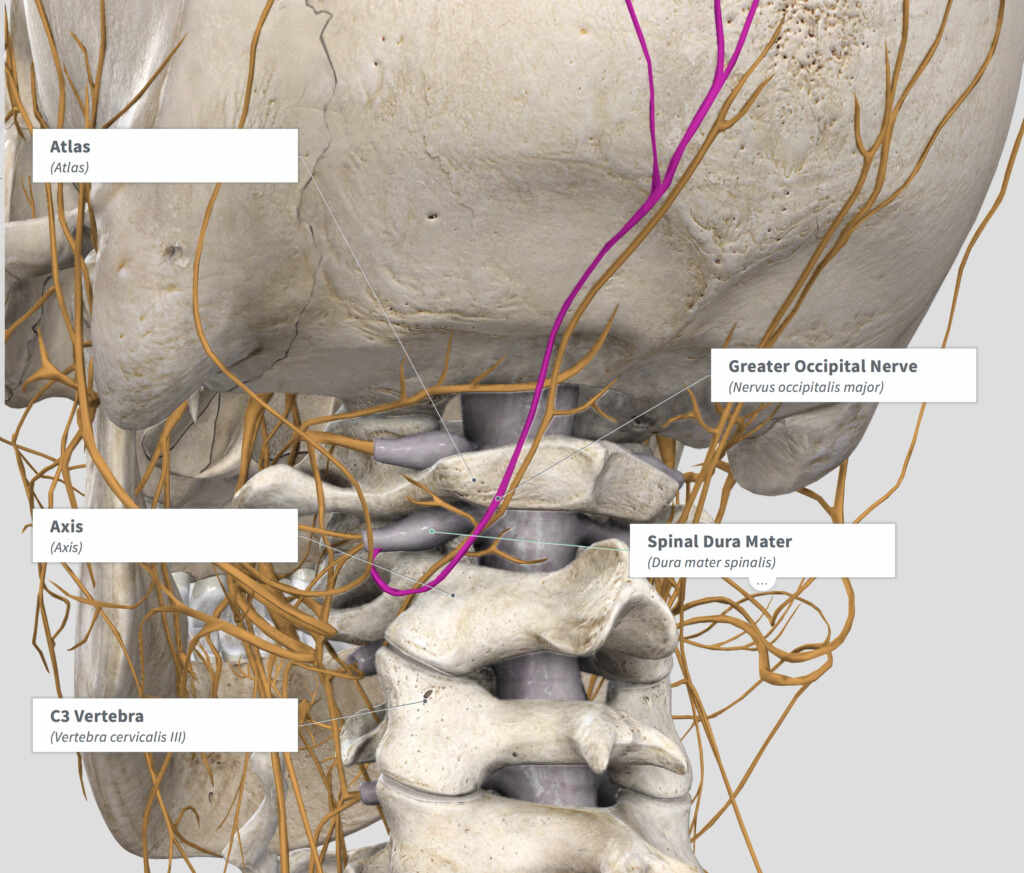
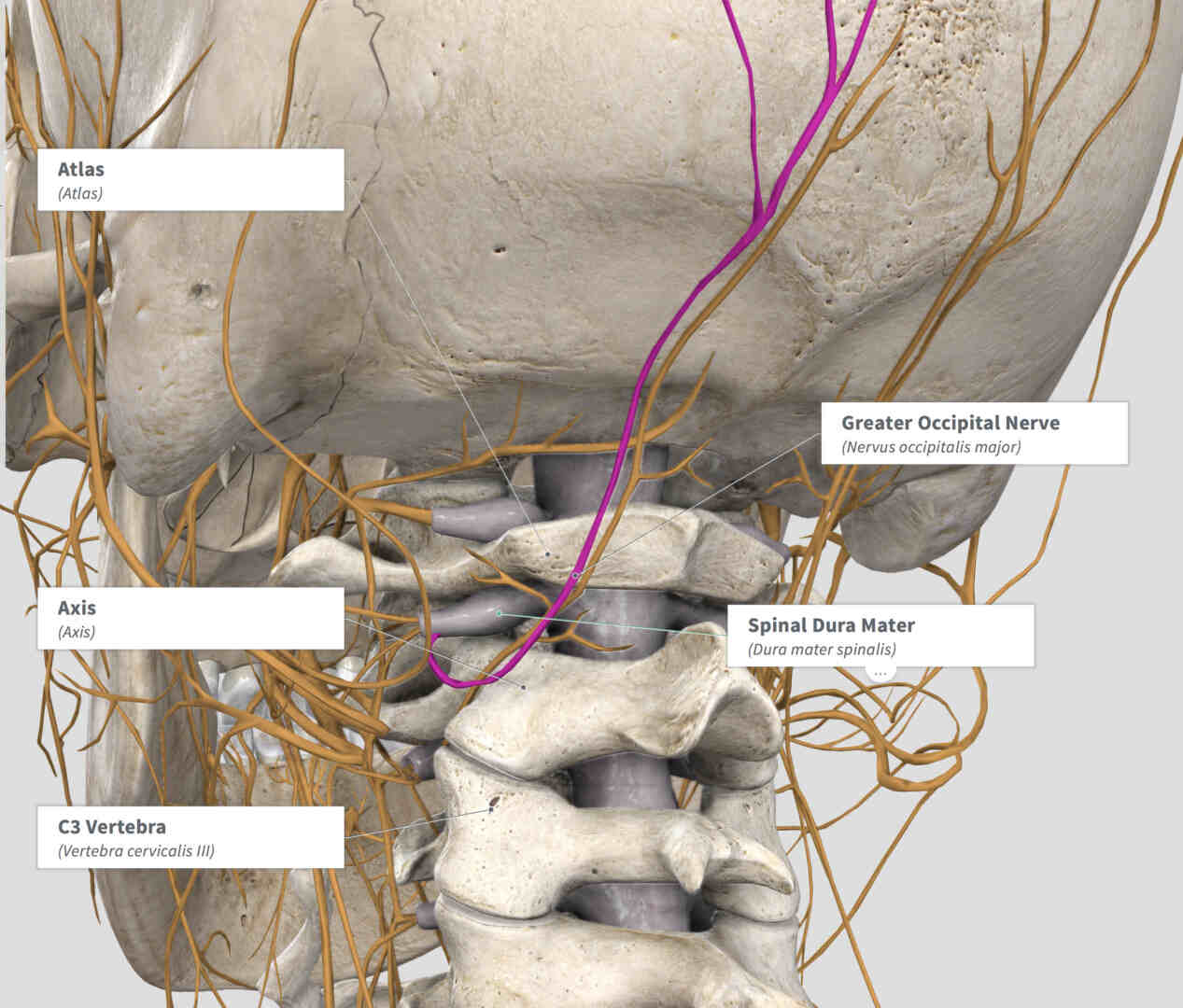
In the accompanying diagram, the Spinal Dura Mater is noted coming out between the spinal bones or vertebrae. This “dura mater” is the coating of the spine and can be thought of as covering these nerve roots that I mention above. When there is cervical spine disease, these nerve roots can be compressed by the spinal vertebrae bones above and below the nerve root. When this happens, many different symptoms can occur depending on which vertebrae and nerve root is involved. A spinal decompression, often called a cervical decompression when performed in the neck region, refers to decreasing the pressure on the nerve root when it emerges from between two vertebrae that are compressing it. This can be done in many ways and is most often performed by a spine surgeon.
What Migraine Surgery Actually Targets
In migraine surgery, we are not working on the nerve root itself, nor on the spine or the bones that make up the spinal column. Microvascular nerve decompression for migraine pain refers to decompressing the actual end nerve, such as the Greater Occipital Nerve seen here in purple. We find that many migraine patients have compression and irritation of these end nerves, also called “peripheral nerves.” Even following cervical decompression, the peripheral nerves are often irritated and continue to cause pain.
Migraine surgery involves finding the nerve that is actually causing the discomfort by using targeted nerve injection mapping, and then operating to remove the compression and irritation formed by surrounding structures such as muscle, blood vessels, or connective tissue. Because we are not operating on the spine or spinal cord, this is very different than cervical spine decompression. Unfortunately many patients with irritation of these peripheral nerves, also called “peripheral neuralgia,” may be misdiagnosed with a nerve root or spinal problem and have cervical decompression fail where peripheral nerve decompression would work well to relieve their pain.
No matter what the cause, a proper workup of migraine pain is important in order to provide the best information and allow that issue to be addressed. If you have had cervical decompression, you may very well still be a candidate for the peripheral nerve decompression performed in migraine surgery. These two operations are completely different and address different issues. I recommend a consultation with a migraine surgeon to discuss your personal history, the symptoms and operations that you have had, and the opportunity to improve your migraine pain with the appropriate treatment.