
Injection Therapy & Nerve Blocks in Santa Barbara, CA
There are a few options for injection therapy for migraine headaches, though the principal two techniques utilize Botox or local anesthesia (lidocaine). In 2010 the FDA approved the use of Botox injections to prevent headaches in chronic migraine patients, and in these patients, Botox is often given as multiple injections around the neck and head for Botox for migraine therapy. The recommended dosing distributes 155 units of Botox divided into 31 different sites, and Botox is routinely successfully used by neurologists and pain control physicians.
When performed by Dr. Lowenstein, these injections are done differently. Dr. Lowenstein performs diagnostic nerve blocks in patients who present to the office with headache pain. These injections provide temporary relief but allow Dr. Lowenstein to pinpoint the cause of the patient’s headache pain, and show us that these patients are good candidates for migraine surgery. If you have a headache when you come to see Dr. Lowenstein, the nerve block is performed with local anesthesia. This injection with Lidocaine and Marcaine can produce immediate though temporary results, indicating that you would be a great candidate for migraine headache surgery.
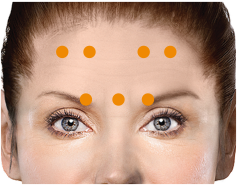
Patients who don’t present to the office with a headache may be treated with migraine Botox using specific point injections to see if there is a reduction in migraine headache symptoms over the course of the next few weeks to months. If your migraine headaches respond to Botox in this injection technique, you are likely a great candidate for migraine headache Botox surgery.
If injections such as these with Botox and/or local anesthesia do not demonstrate any relief of symptoms, you may not be the best candidate for surgery. In these cases, Dr. Lowenstein may recommend a second attempt to make certain that you are not responding. Patients who do not respond to the injection of these nerves should continue to be followed by their neurologist or medical headache specialist. Please contact our team for more information on botox for migraines and botox for headache’s.

The Neurologist/Pain Doctor’s Approach
Pain doctors and neurologists have used Botox to treat and prevent chronic migraines for some time. Their injections are often based on the FDA guidelines which is in turn based on old literature from neurology journals. Per the Botox website, “BOTOX® is injected into shallow muscles, not too deeply beneath the skin. Each treatment involves 31 injections in 7 key areas of the head and neck.”
This injection technique utilizes somewhat of a shotgun approach, injecting small amounts of Botox into lots of areas. Some of these areas may very well be contributing to the patient’s headaches, while others may not. Importantly, however, these “shallow” injections often do not reach the particular muscles that are compressing the nerve- particularly in the back of the neck.

If an injection of a small amount of Botox is even a few millimeters away from a problematic compression point on the nerve, the constricting muscle will remain tight and that nerve will remain irritated. Similarly, the injection of a nerve block agent in the vague region of a problematic nerve may or may not affect the target and therefore may or may not provide desired effects. Additionally, in some cases, it is not muscle causing compression on a nerve, but instead an artery or possibly even some firm tissue or scar. In these cases, the mechanism of Botox may not provide the needed decompression of the nerve even if injected in the region of the problem.
This is NOT to say the medical approach to nerve blocks and the injection of Botox is ineffective—these techniques work for some migraine patients. For those patients who find improvement of their headache pain with this approach, we recommend continuing to have these treatments. If, however, a patient has found that the neurologist’s approach to injections has not improved their headache symptoms, they may still benefit from having a surgeon evaluate them and try a nerve block or Botox therapy in a different manner. As headache botox therapy results will be different for each patient.



The Surgeon’s Approach
So what exactly does this mean? Some patients have had previous nerve blocks or Botox injections by neurologists or pain doctors and have not found relief. This does not mean that a nerve block or Botox injection by a surgeon will be similarly unsuccessful. Dr. Lowenstein’s surgical experience allows him to provide a very specific, directed injection to the problematic region. It should not be surprising that despite previously failed nerve blocks and Botox treatments, a headache patient may find Dr. Lowenstein’s approach remarkably successful. It is important to restate that the purpose of this discussion is NOT to discount the medical or neurologist’s approach to Botox injections which can be effective. Surgeons and medical doctors (such as neurologists and pain doctors) have different experiences and certainly different skill sets which allow each of them to provide different therapies, even when utilizing the same tools- in this case, Botox or local anesthesia. Because a peripheral nerve surgeon has had the experience of actually visualizing the nerves in question as well as the muscles surrounding these nerves in problematic areas, our approach to the use of Botox is more directed to the specific regions where targeted muscle relaxation can decompress the nerve. Dr. Lowenstein’s administration of nerve-blocking agents is based on the detailed anatomic knowledge of the nerve locations.
In the long term, this difference between injection techniques can have very profound implications. Patients who have had previous nerve blocks and Botox injections by other doctors may be mistaken in the belief that they are not candidates for migraine surgery. Until a patient has been evaluated by a surgeon such as Dr. Lowenstein, nerve decompression surgery for occipital neuralgia and migraine headaches should not be ruled out as a potentially life-changing option. The specialized injection approach of the headache Botox surgeon may provide surprising success in patients who have failed injection treatment by other physicians.
FAQs
I’ve had nerve blocks before and they don’t work on me. What makes Dr. Lowenstein different?
It is not at all unusual for us to see patients who have had limited or no success with previous nerve blocks, yet excellent success when Dr. Lowenstein injects them. The advantage of experience in actually seeing the nerves during past operations cannot be overstated, and the detailed knowledge of the anatomy of the nerves allow Dr. Lowenstein to localize the problematic area and treat it precisely.
I have tried Botox before and it did not help. Should I still consider seeing Dr. Lowenstein?
YES! Similar to nerve blocks, Botox must be injected in just the right spot to be effective. A migraine surgeon who is familiar with the nerve’s course as well as the layers of muscle that may be contracting the nerve is more likely to place the Botox in the right spot. Additionally, since most Botox is placed in the classic “crown of thorns” injections around the whole head, a “TIM” injection using Targeted Injection Mapping will allow more precise, specific Botox injections to only the areas that are going to have the greatest effect.
If Botox is not FDA cleared for use in targeted injections, how can you still use it?
Botox can be used in an “off label” application in the manner that migraine surgeons perform their injections. In fact, even for cosmetic uses, Botox is used all over the face when in reality it is only FDA cleared in 2 regions. Botox is actually used for spasm in patients with muscular dystrophy and even in some patients who have some types of gastrointestinal issues. It is also safely used in patients with facial tics, voice disorders, and Parkinson’s disease on an “off label” basis. Dr. Lowenstein’s extensive experience with Botox allows him to explain exactly what to expect and why when using Botox to help with migraine headaches, and you should rest assured that Dr. Lowenstein puts his patient’s safety before everything else.
Why is Dr. Lowenstein so likely to perform a successful injection?
What is the difference between someone who has driven to your house vs someone who is having the directions explained to them? Which of those people are more likely to get there faster without any mistakes? Similarly, Dr. Lowenstein sees the nerves involved in creating migraines on a regular basis, and as such he may be more familiar with how and where they are located. In fact, recent studies of some of the nerves involved in causing migraines have shown that their detailed course through the muscles is not as it has been classically described in anatomy books. A neurologist or pain doctor who has not seen the nerves in previous operative experience may be injecting in the wrong place if their knowledge of the nerves is based only in reading textbooks. It is important to remember that in many if not most cases, neurologist or pain management doctors provide very effective injections. If these injections have failed, however, Dr. Lowenstein’s techniques may still provide pain relief.
Why is Botox only FDA approved for the “ring of thorns” injection around the whole head?
The manner in which Botox was first used involved a “shotgun” type of approach, injecting all over in the hopes that one or more of the injections would have a favorable effect on the compressed nerves. The studies initially submitted to the FDA utilized only this shotgun approach, and when it was found to be safe, the FDA approved it. More targeted injections involve individual areas that Botox is placed to and as the FDA works, studies would need to be performed for each individual site in order to achieve FDA clearnce for injections of this type. Because there are approximately 7 currently known regions that we use Botox in the targeted approach, this would mean the FDA would require 7 times as many studies to clear Botox for use in each of these regions. While those studies are in process, waiting for them to be complete will take a very long time and would prevent the treatment of so many patients who benefit from targeted Botox injections.
How long does Botox for migraines last?
Botox for migraines typically provides relief for about 10-12 weeks. Many patients notice a reduction in headache days within 2-3 weeks of their first treatment.
Am I a candidate for Botox for headaches?
Patients who experience chronic migraines (15 or more headache days per month) may be candidates for Botox. Our specialists will assess your condition to determine if this treatment is right for you.
How is Botox for headaches administered?
The treatment involves a series of small injections in key areas around your head and neck. The process is quick and minimally invasive, usually taking about 15 minutes.
Are there side effects of migraine Botox?
Some patients experience mild swelling, bruising, or discomfort at the injection sites, but these effects are usually temporary. Serious side effects are rare and will be discussed during your consultation.
